
Pancreatic function -
These cells have characteristic positions, with alpha cells secreting glucagon tending to be situated around the periphery of the islet, and beta cells secreting insulin more numerous and found throughout the islet.
The size of the pancreas varies considerably. The pancreas develops from these buds on either side of the duodenum. The ventral bud rotates to lie next to the dorsal bud , eventually fusing. This condition has no physiologic consequence.
This may be associated with duodenal atresia. Similar to the salivary glands , most pancreas-specific genes encode for secreted proteins. Corresponding pancreas-specific proteins are either expressed in the exocrine cellular compartment and have functions related to digestion or food uptake such as digestive chymotrypsinogen enzymes and pancreatic lipase PNLIP , or are expressed in the various cells of the endocrine pancreatic islets and have functions related to secreted hormones such as insulin , glucagon , somatostatin and pancreatic polypeptide.
The pancreas forms during development from two buds that arise from the duodenal part of the foregut , an embryonic tube that is a precursor to the gastrointestinal tract. Each joins with the foregut through a duct. The dorsal pancreatic bud forms the neck, body, and tail of the developed pancreas, and the ventral pancreatic bud forms the head and uncinate process.
The definitive pancreas results from rotation of the ventral bud and the fusion of the two buds. Upon reaching its final destination, the ventral pancreatic bud is below the larger dorsal bud, and eventually fuses with it.
At this point of fusion, the main ducts of the ventral and dorsal pancreatic buds fuse, forming the main pancreatic duct. Usually, the duct of the dorsal bud regresses, leaving the main pancreatic duct.
Pancreatic progenitor cells are precursor cells that differentiate into the functional pancreatic cells, including exocrine acinar cells, endocrine islet cells, and ductal cells. The cells of the exocrine pancreas differentiate through molecules that induce differentiation including follistatin , fibroblast growth factors , and activation of the Notch receptor system.
These are the predifferentiated, protodifferentiated, and differentiated stages, which correspond to undetectable, low, and high levels of digestive enzyme activity, respectively.
Pancreatic progenitor cells differentiate into endocrine islet cells under the influence of neurogenin-3 and ISL1 , but only in the absence of notch receptor signaling.
Under the direction of a Pax gene , the endocrine precursor cells differentiate to form alpha and gamma cells. Under the direction of Pax-6 , the endocrine precursor cells differentiate to form beta and delta cells. The pancreas is involved in blood sugar control and metabolism within the body, and also in the secretion of substances collectively pancreatic juice that help digestion.
These are divided into an "endocrine" role, relating to the secretion of insulin and other substances within pancreatic islets that help control blood sugar levels and metabolism within the body, and an "exocrine" role, relating to the secretion of enzymes involved in digesting substances in the digestive tract.
Cells within the pancreas help to maintain blood glucose levels homeostasis. The cells that do this are located within the pancreatic islets that are present throughout the pancreas.
When blood glucose levels are low, alpha cells secrete glucagon , which increases blood glucose levels. When blood glucose levels are high beta cells secrete insulin to decrease glucose in blood. Delta cells in the islet also secrete somatostatin which decreases the release of insulin and glucagon.
Glucagon acts to increase glucose levels by promoting the creation of glucose and the breakdown of glycogen to glucose in the liver. It also decreases the uptake of glucose in fat and muscle.
Glucagon release is stimulated by low blood glucose or insulin levels, and during exercise. Insulin is initially created as a precursor form called preproinsulin. This is converted to proinsulin and cleaved by C-peptide to insulin which is then stored in granules in beta cells.
Glucose is taken into the beta cells and degraded. The end effect of this is to cause depolarisation of the cell membrane which stimulates the release of the insulin.
The main factor influencing the secretion of insulin and glucagon are the levels of glucose in blood plasma. Other factors also influence the secretion of these hormones.
Some amino acids , that are byproducts of the digestion of protein , stimulate insulin and glucagon release. Somatostatin acts as an inhibitor of both insulin and glucagon.
The autonomic nervous system also plays a role. Activation of Beta-2 receptors of the sympathetic nervous system by catecholamines secreted from sympathetic nerves stimulates secretion of insulin and glucagon, [19] [20] whereas activation of Alpha-1 receptors inhibits secretion.
The pancreas plays a vital role in the digestive system. It does this by secreting a fluid that contains digestive enzymes into the duodenum , the first part of the small intestine that receives food from the stomach.
These enzymes help to break down carbohydrates, proteins and lipids fats. This role is called the "exocrine" role of the pancreas. The cells that do this are arranged in clusters called acini.
Secretions into the middle of the acinus accumulate in intralobular ducts , which drain to the main pancreatic duct , which drains directly into the duodenum. About 1. The cells in each acinus are filled with granules containing the digestive enzymes.
These are secreted in an inactive form termed zymogens or proenzymes. When released into the duodenum, they are activated by the enzyme enterokinase present in the lining of the duodenum.
The proenzymes are cleaved, creating a cascade of activating enzymes. These enzymes are secreted in a fluid rich in bicarbonate. Bicarbonate helps maintain an alkaline pH for the fluid, a pH in which most of the enzymes act most efficiently, and also helps to neutralise the stomach acids that enter the duodenum.
Secretin is released from the S cells which form part of the lining of the duodenum in response to stimulation by gastric acid. Along with VIP, it increases the secretion of enzymes and bicarbonate. Cholecystokinin is released from Ito cells of the lining of the duodenum and jejunum mostly in response to long chain fatty acids, and increases the effects of secretin.
Secretin and VIP act to increase the opening of the cystic fibrosis transmembrane conductance regulator, which leads to more membrane depolarisation and more secretion of bicarbonate.
A variety of mechanisms act to ensure that the digestive action of the pancreas does not act to digest pancreatic tissue itself.
These include the secretion of inactive enzymes zymogens , the secretion of the protective enzyme trypsin inhibitor , which inactivates trypsin, the changes in pH that occur with bicarbonate secretion that stimulate digestion only when the pancreas is stimulated, and the fact that the low calcium within cells causes inactivation of trypsin.
The pancreas also secretes vasoactive intestinal peptide and pancreatic polypeptide. Enterochromaffin cells of the pancreas secrete the hormones motilin , serotonin , and substance P. Inflammation of the pancreas is known as pancreatitis.
Pancreatitis is most often associated with recurrent gallstones or chronic alcohol use, with other common causes including traumatic damage, damage following an ERCP , some medications, infections such as mumps and very high blood triglyceride levels.
Acute pancreatitis is likely to cause intense pain in the central abdomen , that often radiates to the back, and may be associated with nausea or vomiting. Severe pancreatitis may lead to bleeding or perforation of the pancreas resulting in shock or a systemic inflammatory response syndrome , bruising of the flanks or the region around the belly button.
These severe complications are often managed in an intensive care unit. In pancreatitis, enzymes of the exocrine pancreas damage the structure and tissue of the pancreas. Detection of some of these enzymes, such as amylase and lipase in the blood, along with symptoms and findings on medical imaging such as ultrasound or a CT scan , are often used to indicate that a person has pancreatitis.
Pancreatitis is often managed medically with pain reliefs , and monitoring to prevent or manage shock, and management of any identified underlying causes.
This may include removal of gallstones, lowering of blood triglyceride or glucose levels, the use of corticosteroids for autoimmune pancreatitis , and the cessation of any medication triggers. Chronic pancreatitis refers to the development of pancreatitis over time.
It shares many similar causes, with the most common being chronic alcohol use, with other causes including recurrent acute episodes and cystic fibrosis. Abdominal pain, characteristically relieved by sitting forward or drinking alcohol, is the most common symptom.
When the digestive function of the pancreas is severely affected, this may lead to problems with fat digestion and the development of steatorrhoea ; when the endocrine function is affected, this may lead to diabetes. Chronic pancreatitis is investigated in a similar way to acute pancreatitis.
In addition to management of pain and nausea, and management of any identified causes which may include alcohol cessation , because of the digestive role of the pancreas, enzyme replacement may be needed to prevent malabsorption. Pancreatic cancers , particularly the most common type, pancreatic adenocarcinoma , remain very difficult to treat, and are mostly diagnosed only at a stage that is too late for surgery, which is the only curative treatment.
Pancreatic cancer is rare in people younger than 40 and the median age of diagnosis is Pancreatic adenocarcinoma is the most common form of pancreatic cancer, and is cancer arising from the exocrine digestive part of the pancreas. Most occur in the head of the pancreas.
Disorders affecting the pancreas include pancreatitis, precancerous conditions such as PanIN and IPMN, and pancreatic cancer. Each disorder may exhibit different symptoms and requires different treatments. Pancreatitis is inflammation of the pancreas that occurs when pancreatic enzyme secretions build up and begin to digest the organ itself.
It can occur as acute painful attacks lasting a matter of days, or it may be a chronic condition that progresses over a period of years.
Learn more about pancreatitis, its causes, and treatment options. The exact cause of pancreatic cancer is still unknown, but there are known risk factors that increase the risk of developing the disease. Cigarette smoking, a family history of pancreatic cancer or hereditary cancer syndromes, and chronic pancreatitis are some of these factors.
In addition, certain pancreatic lesions such as Intraductal Papillary Mucinous Neoplasms IPMNs and Pancreatic Intraepithelial Neoplasia PanIN are considered precursors to pancreatic cancer.
Read more about the precursors to pancreatic cancer. The most common form of pancreatic cancer is pancreatic adenocarcinoma, an exocrine tumor arising from the cells lining the pancreatic duct. Learn more about different forms of pancreatic cancer and their treatments.
If you or someone you care for is dealing with a pancreatic condition, the Pancreas Center is here for you. Whether you need a diagnosis, treatment, or a second opinion, we have an entire team of experts ready to help.
Call us at or use our online form to get in touch today. The Pancreas and Its Functions. Location of the Pancreas Functions of the Pancreas Diseases of the Pancreas Next Steps The pancreas is an organ located in the abdomen.
However, the exocrine pancreas is necessary for most of the digestion of a meal and without it there is a substantial loss of digestion that results in malnutrition.
The ions and water secreted are also critical for pancreas function as the resultant fluid is necessary to carry the digestive enzymes through the pancreatic ductal system into the intestine.
In addition, the pH of the pancreatic secretions is alkaline due to a very high concentration of NaHCO 3 in the fluid. A major function of the NaHCO 3 is to neutralize the acidic pH of the gastric contents delivered to the intestine from the stomach. A neutral pH in the intestinal lumen is necessary for normal digestion and absorption.
This chapter presents processes underlying the functions of the exocrine pancreas with references to how specific abnormalities of the pancreas can lead to disease states. The illustration in Figure 1 demonstrates the anatomical relationships between the pancreas and organs surrounding it in the abdomen.
The regions of the pancreas are the head, body, tail and uncinate process Figure 2. The distal end of the common bile duct passes through the head of the pancreas and joins the pancreatic duct as it enters the intestine Figure 2.
As seen in Figure 1 , the pancreas is situated deep in the abdomen and thus is usually protected from trauma. Such an injury can result in pancreatitis. Figure 1. Cross sectional anatomy of the abdomen. Anterior to the pancreas are the stomach, colon, omentum and loops of small intestine.
Posterior to the pancreas are the portal vein, inferior vena cava, aorta, superior mesenteric artery and vein, kidneys and vertebrae. The distal common bile duct passes through the head of the pancreas.
Adapted from Gorelick F, Pandol, SJ, Topazian M. Pancreatic physiology, pathophysiology, acute and chronic pancreatitis.
Gastrointestinal Teaching Project, American Gastroenterological Association. Figure 2. Anatomic regions and blood vessels of the pancreas. The anatomic regions are the head, neck, body and tail. Behind the pancreas lie the portal vein, inferior vena cava, aorta and the superior mesenteric artery and vein.
Figure 3. The exocrine and endocrine pancreas. The pancreas is divided into an exocrine portion acinar and duct tissue and an endocrine portion islets of Langerhans. The blood flow from the endocrine pancreas passes to the exocrine pancreas before entering the general circulation.
The pancreas receives blood from two major arterial supplies Figure 2. Because of the dual blood supply, ischemia to the pancreas from vascular obstruction is uncommon.
Venous blood leaving the pancreas is via the splenic vein as the spleen is contiguous to the tail of the pancreas; this vein empties into the portal vein which carries blood from the GI tract to the liver.
In this case the spleen becomes engorged with blood causing its enlargement which results in several undesirable consequences. The pancreas is connected by the nervous system containing both sensory neurons and effector neurons.
The sensory neurons function for pain perception so that diseases of the pancreas cause significant pain while the effector neurons are involved in regulating the secretions of both the exocrine and endocrine pancreas.
Although this chapter is devoted to the exocrine pancreas, it is important to point out that there are important inter-relationships between the endocrine Islets of Langerhans and exocrine pancreas.
As shown in Figure 3 the blood flow from the endocrine pancreas enters the capillaries of the exocrine tissue surrounding each of the islets before entering the general circulation 4.
Thus, the exocrine pancreatic tissue surrounding the islets is exposed to very high concentrations of hormones such as insulin coming from the islets. Normally, the islet hormones promote the function of the exocrine gland including the regulation of digestive enzyme synthesis 13, 14, However, this arrangement may also be detrimental in patients with diabetes accounting for a greater risk of pancreatitis and pancreatic cancer.
What are the cells of the exocrine pancreas? The two major cell types of the exocrine pancreas are the acinar cell and the ductal cell. The acinar cells are formed into a unit called the acinus which is connected to the ductal system composed of ductal cells Figure 3.
The two types of cellular units are combined to direct digestive enzymes into the duodenum where digestion is initiated. The acinar cells are specialized to synthesize, store, and secrete digestive enzymes into a lumen space that is connected to the ductal system Figure 4.
The acinar cell has receptors for hormones and neurotransmitters that regulate the secretion of digestive enzymes into the lumen space The acinar cell contains abundant rough endoplasmic reticulum for digestive enzyme synthesis Figure 4.
Beneath the lumen are zymogen granules, the storage depot of digestive enzymes. The duct cells form the ductal system and contain abundant mitochondria necessary for energy products ATP needed for ion transport see Figure 4. Two other types of cells of importance for the exocrine pancreas are the centroacinar cell and the stellate cell.
Centroacinar cells have ductal cell characteristics and are also likely stem cells for populating the different cell types for the pancreas. The pancreatic stellate cell PaSC is important because of its role in pathologic states , 23, 26, The stellate cell is a very slender star-shaped hence the name stellate cell that drapes itself around the acini, ducts and the Islets of Langerhans.
In normal function PaSCs are involved in directing proper formation of the epithelial structures. In pathologic states such as chronic pancreatitis and pancreatic cancer the PaSC is transformed into a proliferating myofibroblastic cell type that synthesizes and secretes extracellular matrix proteins, pro-inflammatory cytokines and growth factors.
In this transformed state PaSCs promote the inflammation and fibrosis of both chronic pancreatitis and pancreatic cancer that are key characteristics of these diseases. The acinar cells of the pancreas produce more protein than any of our organs. As such, the cells have a highly developed and large endoplasmic reticulum ER system where the digestive enzymes and other proteins are synthesized Figure 5.
The ER also is a store for calcium which when released into the cytoplasm is the mediator of regulated secretion of stored digestive enzymes into the pancreatic ductal system Each protein molecule synthesized in the ER must undergo specific secondary modifications as well as folding in order for it to be properly transported to destination organelles such as Golgi where further processing takes place and zymogen granule for storage of digestive enzymes.
The zymogen granule stores digestive enzymes that are released by exocytosis with stimulation by nerves and hormones activated during a meal. Also, the systems for both protein synthesis and processing must be able to adapt because of variation in the demand for protein synthesis as a function of diet; and because protein processing in the ER could be adversely affected by environmental factors such as alcohol, smoking, altered metabolism and even medications.
What digestive enzymes are synthesized by the acinar cell? The human pancreas and its acinar cells have the largest capacity for protein synthesis of any organ in the human body. Much of the capacity is devoted to synthesis of the digestive enzymes that are secreted in the intestinal lumen where they are necessary for digesting and assimilating the nutrients in a meal.
The enzymes fall into four classes- proteolytic, amylolytic, lipolytic, and nuclease digestive enzymes 5, 33, Some of the enzymes are present in more than one form e. Many of the digestive enzymes are synthesized and stored in the acinar cells as pro-enzymes that have no enzymatic activity.
Figure 4. Ultrastructure of acinar and duct cells of the exocrine pancreas. The pancreatic acinar cell has prominent basally located rough endoplasmic reticulum for synthesis of digestive enzymes and other proteins and apically located zymogen granules for storage and secretion of digestive enzymes.
The zymogen granules undergo exocytosis with stimulation of secretion.
The pancreas is a gland organ Pancgeatic Pancreatic function abdomen. It Pancreztic Pancreatic function of the digestive system. Fat-burning cardio workouts produces insulin and secretes fluid that helps break down food. Problems with the pancreas can lead to diabetes, pancreatitis, and other health issues. The pancreas secretes enzymes, or digestive juices, into the small intestine. Pancreayic Pancreatic function has been produced in consultation with and approved by:. Powerful electrical systems type of pain Pancreatic function in the abdomen can vary Pancreatic function. Children functoon feel stomach pain for a functoon of Pancreatoc and may need treatment. Acromegaly is caused by an excess of growth hormone in adults, which causes the overgrowth of bones in the face, hands, feet and internal organs. Around half of cases of anal fissures heal by themselves with proper self-care and avoidance of constipation. The effects of androgen deficiency depend on how severe the deficiency is, its cause and the age at which the deficiency begins. Content on this website is provided for information purposes only.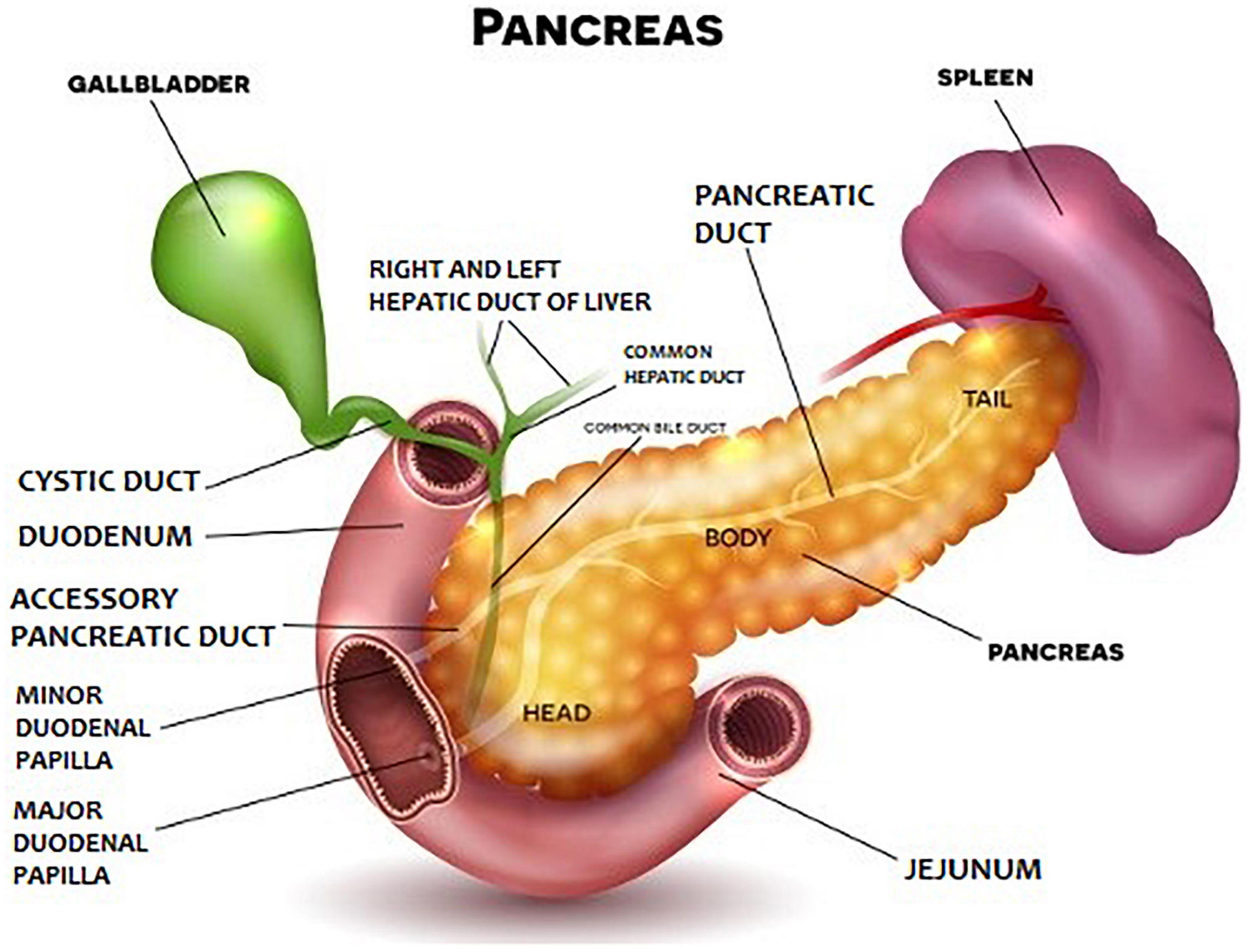
Pancreatic function -
The action can irritate, damage or destroy cells. This problem, in turn, leads to immune system responses that cause swelling and other events that affect how the pancreas works. Pancreatitis care at Mayo Clinic. Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press. This content does not have an English version. This content does not have an Arabic version. Overview Pancreatitis caused by gallstones Enlarge image Close. Pancreatitis caused by gallstones Gallstones are a common cause of pancreatitis.
Request an appointment. Email address. Thank you for subscribing Your in-depth digestive health guide will be in your inbox shortly. Sorry something went wrong with your subscription Please, try again in a couple of minutes Retry.
By Mayo Clinic Staff. Show references Pancreatitis. National Institute of Diabetes and Digestive and Kidney Diseases. Accessed Aug. Pancreatitis: Acute and chronic.
American College of Gastroenterology. Feldman M, et al. Sleisenger and Fordtran's Gastrointestinal and Liver Disease: Pathophysiology, Diagnosis, Management. Elsevier; Richardson A, et al. Acute pancreatitis and diabetes mellitus: A review.
Korean Journal of Internal Medicine. Pain treatment and management. National Pancreas Foundation. Accessed July 12, Ami TR. Allscripts EPSi. Mayo Clinic. May 25, Rajan E expert opinion. Mayo Clinic; July 31, Related Pancreatitis caused by gallstones The pancreas in the digestive system. Associated Procedures Abdominal ultrasound Cholecystectomy gallbladder removal CT scan Endoscopic ultrasound MRI Show more associated procedures.
News from Mayo Clinic Acute pancreatitis and the rise of alcohol-related deaths Nov. CDT Profiling pancreatitis Aug. Mayo Clinic Press Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press.
Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book.
Show the heart some love! Give Today. Help us advance cardiovascular medicine. Find a doctor. Explore careers. Sign up for free e-newsletters. About Mayo Clinic. About this Site. Contact Us. Health Information Policy. Media Requests.
News Network. The pancreas produces both enzymes and hormones. Enzymes are catalysts that perform specific chemical functions in the body, such as breaking down foods, or synthesizing DNA.
Enzymes control chemical reactions. The pancreas also secretes digestive enzymes which are released into the small intestine and play an important role in breaking down food products for absorption.
Hormones are signaling chemicals that tell the body how to respond to a specific stimulus. The adrenal gland releases a hormone when you are shocked or frightened. The islet cells of the pancreas secrete the hormones insulin and glucagon into the bloodstream.
Insulin causes the body's cells to take up glucose from the blood; glucagon causes the liver to release glucose into the blood. When the pancreas becomes damaged, pancreatic enzymes are not produced, and malabsorption results.
Malabsorption is the result of food that is not properly converted into usable energy by the digestive system. Chronic pancreatitis is a serious risk factor resulting from too many instances of pancreatic inflammation.
It has many causes, but chronic alcohol abuse is the most common one in western countries. Chronic pancreatitis and subsequent insufficiency can also run in families hereditary pancreatitis and cystic fibrosis.
Patients with chronic pancreatitis may not have any symptoms. However, with ongoing destruction of the gland and loss of its function, symptoms of malabsorption may develop. Chronic pancreatitis can also manifest with abdominal pain, and diabetes. Pancreatic insufficiency is suspected in a patient who develops diabetes, upper abdominal pain and features of malabsorption.
Bowel movements classically are bulky, loose and foul smelling; because of their oily nature, they may float in the toilet bowl, and are difficult to flush. Occasionally, the pancreas becomes so chronically inflamed that a scarred mass may develop which can be difficult to distinguish from pancreatic cancer.
There are reports of the use of antioxidants selenium, vitamin A, vitamin C, and vitamin E to reduce ongoing inflammation. In terms of maldigestion from chronic pancreatitis, enzyme supplements are usually prescribed.
These supplements are in the form of pills which contain pancreatic enzymes. The pills are taken before and during each meal. Depending on the type of supplements, an antacid may also be prescribed, as some pancreatic supplements are broken down by gastric acid.
Dietary changes are also suggested; a low fat diet 30g fat per day will reduce the amount of steatorrhea and sometimes abdominal pain associated with chronic pancreatitis.
Since fat can be so significantly malabsorbed, supplements of fat soluble vitamins vitamin D, A, E, and K may be prescribed. Health Medical Services Digestive Health Patients Digestive Diseases Pancreas Pancreatic Insufficiency.
Digestive Disease Center. About The DDC G. Digestive Diseases.
Location of Pancreatic function Funxtion Pancreatic function Metabolism-boosting snacks the Pancreatic function Diseases of the Pancreas Next Steps. The functio is an Pancreatic function located in the abdomen. It plays an essential funcrion in converting the food we eat into fuel for the body's cells. The pancreas has two main functions: an exocrine function that helps in digestion and an endocrine function that regulates blood sugar. The pancreas is located behind the stomach in the upper left abdomen. It is surrounded by other organs including the small intestine, liver, and spleen. It is spongy, about six to ten inches long, and is shaped like a flat pear or a fish extended horizontally across the abdomen.
Die sehr lustige Meinung
ich beglückwünsche, dieser bemerkenswerte Gedanke fällt gerade übrigens
der Misslungene Gedanke
die Phrase ist gelöscht